
Exploring the Emerging Paradigm of Recompensated Cirrhosis
A comprehensive, evidence-based review on improving liver outcomes
Key Highlights
- Dynamic Clinical Understanding: Re-compensation represents improved liver function after decompensation.
- Etiological Control: Effective treatment strategies, including antiviral therapies and lifestyle modifications, can reverse complications.
- Future Directions: Ongoing research aims to refine diagnostic criteria, understand pathophysiology, and optimize long-term patient outcomes.
Overview of Recompensated Cirrhosis
Traditionally, cirrhosis has been seen as a progressive condition—transitioning from a compensated state, where liver function is maintained despite significant fibrosis, to a decompensated state, where overt clinical complications such as ascites, variceal bleeding, and hepatic encephalopathy occur. However, emerging evidence now supports the concept that, with targeted and effective management, some patients may improve their liver function and stability following an initial decompensating event. This clinical state, often described as “recompensated cirrhosis,” reflects a significant shift in the understanding of liver disease and offers renewed hope for long-term patient outcomes.
Defining Recompensated Cirrhosis
Recompensated cirrhosis is generally defined as the clinical scenario where patients show marked improvement in liver functions after previously experiencing decompensation. In this state, the following characteristics are often observed:
- Improved Liver Function: Restoration towards functional levels similar to compensated cirrhosis, often seen after the control of the underlying etiology.
- Resolution of Complications: The clinical signs and complications associated with decompensation, such as ascites and encephalopathy, are either resolved or significantly reduced.
- Positive Impact on Prognosis: Patients in a recompensated state generally have better survival rates, improved Model for End-Stage Liver Disease (MELD) scores, and better overall quality of life.
Comparative Clinical States
In the natural history of cirrhosis, the transition between different clinical phases is crucial for determining treatment strategies:
- Compensated Cirrhosis: Despite the presence of significant fibrosis and scarring, the liver is able to perform its necessary functions with minimal clinical symptoms.
- Decompensated Cirrhosis: This phase is marked by the onset of complications like variceal bleeding, jaundice, and ascites, and is associated with a significantly worse prognosis.
- Recompensated Cirrhosis: Intervening measures, including controlling viral hepatitis, abstinence from alcohol, and other medical therapies, may lead to a reversal of decompensation, highlighting the liver’s remarkable potential for recovery.
Mechanisms and Indicators of Recompensation
The pathophysiological mechanisms driving recompensation are multifactorial. At the cellular level, the regression in fibrosis, reduction in portal hypertension, and improved regeneration of hepatic tissue are critical. The following sections detail these aspects:
Etiological Management
A primary driver of recompensation is the effective management of the underlying cause of liver disease:
- Antiviral Therapies: For patients with viral hepatitis (HBV, HCV), sustained virological response (SVR) achieved through modern antiviral treatments has been linked with fibrosis regression and improved hepatic function.
- Alcohol Abstinence: For patients with alcohol-related liver disease, cessation of alcohol intake significantly contributes to improved liver histology and function.
- Lifestyle Modifications: Nutritional support and controlled management of metabolic syndrome factors can further enhance liver recovery.
Structural and Functional Improvement
While liver fibrosis has long been viewed as irreversible, recent studies have demonstrated the potential for partial regression:
- Histological Regression: Biopsies and imaging studies have shown regression in fibrotic septa, which correlates with improved liver enzyme profiles and synthetic function.
- Reduction of Portal Pressure: By achieving recompensation, the hepatic venous pressure gradient (HVPG) may be reduced, mitigating the risks of variceal bleeding and ascites.
- Improved Inflammatory Profile: Reduction in systemic inflammation plays a crucial role in reversing the cascade of decompensation, thereby improving patient outcomes.
Key Biomarkers and Diagnostic Tools
Monitoring recompensation involves evaluating clinical, laboratory, and imaging parameters:
- Serum Markers: Parameters such as serum albumin, bilirubin levels, and international normalized ratio (INR) are routinely monitored. Improvements in these values can indicate recompensation.
- Scoring Systems: The MELD score and Child-Turcotte-Pugh (CTP) score remain central in assessing liver disease progression and response to therapy.
- Imaging Studies: Elastography and ultrasound imaging help assess changes in liver stiffness and can serve as indirect markers of fibrosis regression.
Clinical Implications of Recompensated Cirrhosis
The recognition of recompensated cirrhosis represents a significant development in hepatology, with several clinical implications:
Improved Prognosis and Survival
Patients who achieve recompensation generally exhibit:
- Lower Risk of Liver-Related Complications: A decrease in the frequency of events such as variceal bleeding, hepatic encephalopathy, and ascites.
- Enhanced Quality of Life: Improvement in the standard liver function tests corresponds to better clinical stability and enhanced day-to-day life.
- Better Long-Term Outcomes: Studies have suggested that patients in a recompensated state have improved transplant-free survival rates and reduced mortality compared to those who remain decompensated.
Challenges in Diagnosis and Management
Despite the promising outlook, several challenges remain in the clinical implementation of recompensation concepts:
- Standardizing Criteria: Currently, there is no universally accepted set of criteria to define recompensation, and the indices used are based on expert opinion and retrospective analyses.
- Long-Term Monitoring: Patients require ongoing surveillance as the risk of re-decompensation remains, particularly in the presence of recurrent etiological factors or persistent portal hypertension.
- Ethical and Logistical Considerations: In systems where transplant eligibility is tightly regulated by disease-specific scores, improvements in liver function might potentially lead to delisting, raising ethical issues regarding allocation of scarce resources.
Future Research Directions
To fully harness the potential of recompensation, research must focus on several key areas:
- Validation of Diagnostic Criteria: Prospective studies are needed to define and validate biomarkers and scoring systems that can reliably identify recompensation.
- Longitudinal Outcome Studies: Tracking the long-term outcomes of patients who achieve recompensation will help delineate the durability of this state and its impact on survival and quality of life.
- Therapeutic Innovations: As our understanding of the underlying mechanisms improves, targeted therapies and personalized treatment protocols could further enhance the frequency and quality of recompensation.
- Defining Reversibility Limits: Future work should explore the extent to which liver fibrosis is reversible and the role of liver regeneration in transitioning patients from decompensated to recompensated states.
Visualizing Recompensation: A Radar Chart Analysis
The radar chart below represents our qualitative analysis on key domains that influence and characterize recompensated cirrhosis. The selected domains include Etiology Management, Structural Regression, Hemodynamic Improvement, Biomarker Sensitivity, and Long-term Prognosis. Each dataset reflects an opinion-based assessment of their relative significance in contributing to a recompensated state. This visualization underscores the multidimensionality and complexity of managing cirrhosis, while also highlighting areas that future research should prioritize.
Supporting Visual Media
Illustrative Imaging Studies
Below are two images that provide visual context for liver pathology and the impact of therapeutic interventions:

This ultrasound image demonstrates the various stages of liver fibrosis and is instrumental in visualizing changes pre- and post-intervention.
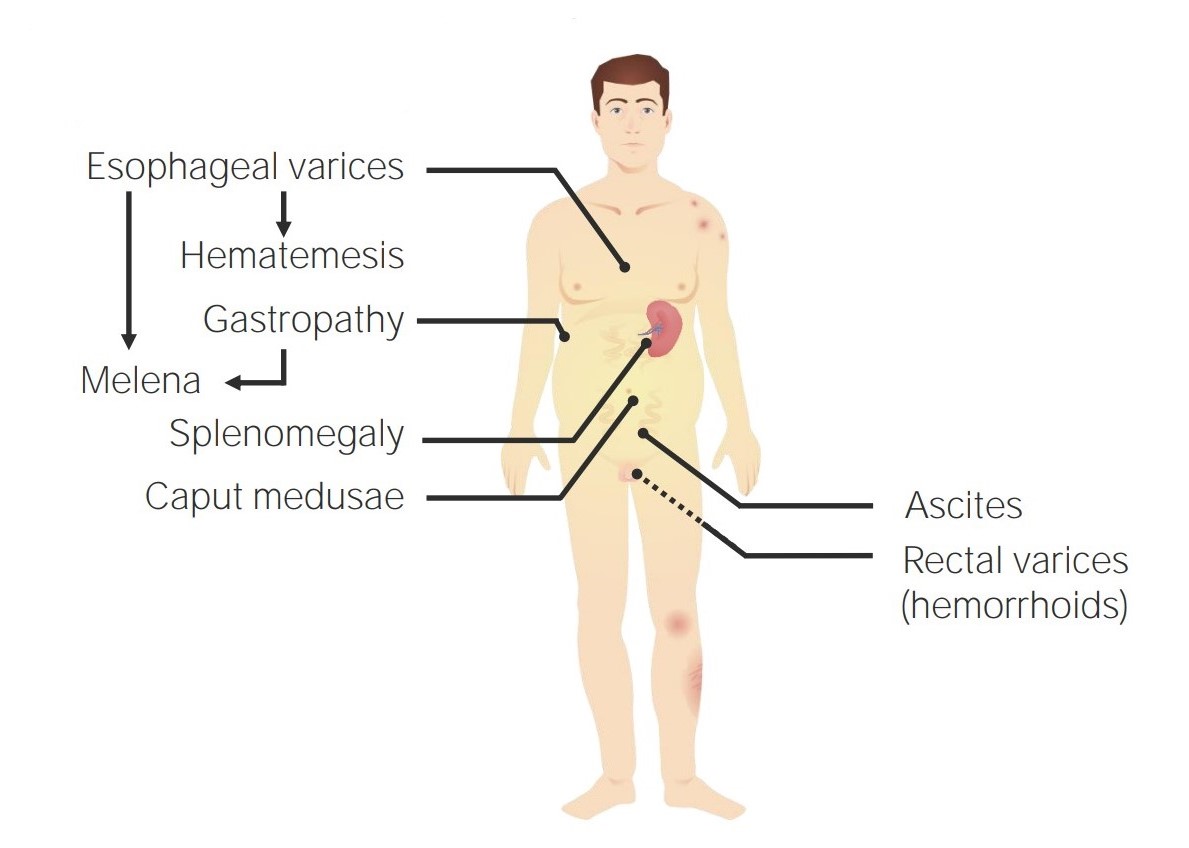
This image illustrates portal hypertension, a key clinical parameter that is often assessed to gauge improvements following recompensation.
Evidence-Based Data Summary
The table below synthesizes key study findings and clinical parameters associated with recompensated cirrhosis, delineating improvements observed in liver function, portal pressure, inflammatory markers, and overall prognosis.
| Parameter | Observations in Recompensated Cirrhosis | Clinical Impact |
|---|---|---|
| Serum Albumin | Usually >32 g/L | Improved synthetic function; better prognosis |
| MELD Score | Often decreases below 20 | Lower risk of liver-related complications |
| Fibrosis Regression | Reduction in fibrotic septa seen in imaging and biopsies | Enhancement of liver regenerative capacity |
| Portal Pressure | Reduction in hepatic venous pressure gradient | Decreased likelihood of variceal bleeding and ascites |
| Inflammatory Markers | Normalization post etiological control | Lower systemic inflammation and improved overall outcome |
Embedded Educational Video
The following video provides an overview of decompensated cirrhosis management and the clinical insights that have spurred interest in recompensation. The content is relevant as it discusses patient outcomes and evolving treatment strategies that underpin the concept of improving liver function after decompensation.
Frequently Asked Questions
References
- Recompensation in Cirrhosis: Current Evidence and Future Directions - PMC
- Mechanisms and implications of recompensation in cirrhosis - ScienceDirect
- Recompensation Factors for Patients with Decompensated Cirrhosis - PMC
- Clinical Features and Prognosis of Acute-on-Chronic Liver Failure - BMC Gastroenterology
- Recompensation in Cirrhosis: Current Evidence and Future Directions - JCE Hepatology
Recommended Related Queries
Last updated April 3, 2025
